Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Research Article(ISSN: 2641-1687) 
Is Silodosin a better Alternative to Tamsulosin as A Part of Medical Expulsion Therapy in patients with Lower Ureteric Calculi: A Comparative Study? Volume 3 - Issue 4
Mishra RP1, Chandra Arun2*, Vishal Bulla3, Alok1, Ahmad Imran3, Srivastava SK2
- 1MBBS, DNB Junior Resident 3rd Year General Surgery, India
- 2MBBS, M.S (General Surgery), Senior Consultant, India
- 3Department of Urology, Tan Tock Seng Hospital, Singapore
Received: February 01, 2022; Published: July 06, 2022
Corresponding author: Chandra Arun, MBBS, MS, Senior Consultant, Department of General Surgery (Urology Division), RML Hospital, Gomti Nagar, India
DOI: 10.32474/JUNS.2022.03.000169
Abstract
Aim: To evaluate the efficacy of Silodosin over Tamsulosin in treatment of uncomplicated lower ureteric calculi.
Material and Methods: A prospective, randomized controlled study was conducted in the Department of General Surgery Dr RML Hospital Lucknow India, from April 2014 to Dec 2015, 158 patients who were between the age group of 21 –55 years, who had unilateral, uncomplicated lower ureteric stones ≤10mm were registered after ethical clearance and were divided into two groups. Group A received Silodosin (8mg) daily, whereas Group B received Tamsulosin (0.4mg) daily for a maximum period of 6 weeks. The patients were reviewed fortnightly with radiological studies. The primary bottom-line was the stone expulsion rate and the secondthe stone expulsion time.
Results: A spontaneous stone expulsion was observed in 65 of the 74patients (87.8%) in Group A and in 49 of the out 76 patients (64.4%) in group B. The stone expulsion rate was significantly higher in Group A than in Group B (p < 0.05). There was also a significant difference between the groups with regards to the mean stone expulsion time. The mean expulsion time was 10.5±3.5 days in Group A vs. 16.5±7.5 days in Group B (p <0.05).
Conclusion: With the above results, Silodosin was found to be clinically way superior to Tamsulosin, both in view of the stone expulsion rate and time.
Keywords: Medical Expulsion Therapy; Lower Ureteric calculi; Silodosin; Tamsulosin
Introduction
Stone disease is one of the most common afflictions of the modern society and it has been described since antiquity. As it has been estimated that 50% of the patients will have a recurrence of colic within 5 years of their first episodes. Urolithiasis is a chronic disease with substantial economic consequences and a great public health importance [1,2]. Ureteric stones constitute 20% of all urinary tract stones and 70% of all ureteric stones are located in the distal ureter [3]. Although ureteral stones less than 10 mm in diameter spontaneously expulse in a significant percentage of patients without any intervention [4], they can lead to serious problems without appropriate medical attention. Deficiency of and complications with treatment options such as extracorporeal shock wave lithotripsy (ESWL), ureteroscopy (URS), and open/ laparoscopic ureter lithotomy have become concerns with the treatment of ureteral stones. These concerns in addition to the high rate of spontaneous expulsion of ureteral stones have led the use of drug therapies that could facilitate stone clearance to become a primary consideration. Of the many drugs that have been tested for medical expulsive therapy (MET) in the treatment of ureteral stones, alpha blockers and calcium channel blockers (CCBs), specifically Nifedipine, are the only treatment modalities for which sufficient data have been collected [5]. Of these modalities, alpha blockers have been found superior to CCBs in terms of the stone expulsion rate and side effect profile [6,7]. Alpha blockers are thus recommended by the American Urological Association (AUA) and the European Association of Urology (EAU) for MET of distal ureteral stones less than 10 mm in diameter [8,9].
There has been a paradigm shift in the management of the ureteric calculi in the past decade, with the introduction of lesser invasive methods and newer drugs. The alpha1–blockers which were first developed as anti–hypertensive drugs, are now being effectively used in the management of benign prostatic hyperplasia, due to their relaxing properties on the urinary tract. Recent studies have reported excellent results with the medical expulsion therapy for the lower ureteric calculi, with alpha1 blockers. Their use in the treatment of lower ureteric stones arose from the concept that they could induce a selective relaxation of the ureteric smooth muscle, which could inhibit the ureteric spasms and result in dilatation of the ureteral lumen. There is a large body of published data which have shown the efficacy of such a therapy in increasing the expulsion rate and in decreasing the expulsion time of the stones [10-14]. Their use has thus become an accepted practice. Tamsulosin, an α1-adrenoceptor antagonist, is one of the most popular and effective medical agents, which is used for the expulsive therapy. Silodosin, a recently introduced selective α(1A)-adrenoceptor antagonist, has shown promising results with fewer side effects and a better efficacy. There are very few studies comparing Silodosin & Tamsulosin. Here in this study, we want to evaluate the efficacy of Silodosin over Tamsulosin in treatment of uncomplicated lower ureteric calculi.
Materials and Methods
A prospective and a randomized controlled study was conducted in the Department of General Surgery (Urology Division) Dr RML Hospital Lucknow India, from April 2014 to Dec 2015, a total of 158 patients (M=72; F=86) who were between age group of 21–55 years, who had unilateral, non–impacted, uncomplicated lower ureteral stones which were ≤10mm, were registered in a prospective study after ethical clearance and they were randomized into two groups. The sample size of the study was arbitrarily determined, and it was not based on the statistical calculations. The patients were evaluated with plain X–ray KUB, ultrasonography and noncontrast computed tomography (NCCT) scans whenever they were necessary. The stone size was calculated on the first plain X–ray KUB or NCCT KUB by using a digital ruler and the largest dimension of the stone was considered as the stone size. All the patients provided informed written consents and they were properly informed about the study in which they would be registered.
The patients were randomized into two treatment groups of 79 patients each, by using a random number table. Group A received Silodosin (8 mg) daily, whereas Group B received Tamsulosin (0.4 mg) daily, for a maximum period of 6weeks.Five patients in group A and three patients in group B did not turn up for review, hence our study continued with 74 patients in group A and 76 in group B. Every patient was prescribed Diclofenac sodium 100 mg tablet as required for pain relief. The patients were advised that on experiencing an episode of unbearable ureteric colic and expulsion of stone, they should immediately report to us over telephone. The patients were followed up fortnightly with X–rays KUB region and ultrasonography. The patients were instructed to note the date and time of the stone passage. The patients were followed up until they were rendered stone-free by intervention or spontaneous stone expulsion, as was confirmed by the patient, for a maximum of 6 weeks. The primary bottom-line was the stone expulsion rate and the second was the stone expulsion time, the rates of the interventions such as ureter lithotripsy, extracorporeal shock wave lithotripsy, or ureteral stenting, unbearable ureteric colic and side effects. The expulsion time was defined as the number of days from the randomized date to the stone expulsion date.
Results
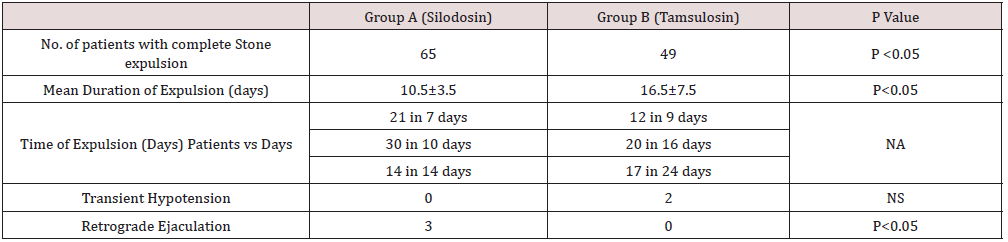
There was no significant difference in base line characteristics of the study groups (Table 1). A spontaneous stone expulsion was observed in 65 of the 74patients (87.8%) in Group A and in 49 of the out 76 patients (64.4%) in group B. The stone expulsion rate was significantly higher in Group B than in Group A (p < 0.05). There was also a significant difference between the groups with regards to the mean stone expulsion time (P< 0.05). The mean expulsion time was 10.5±3.5 days in Group A vs. 16.5±7.5 days in Group B (Table 2).
Side effect profile in our study
Three of the male patients who took Silodosin experienced a retrograde ejaculation but a lower incidence of the side effects which were related to the peripheral vasodilatation as compared to the patients who took Tamsulosin. The patients who experienced a retrograde ejaculation were followed-up after the completion of the study and they were found to have been relieved of this problem. No side-effects that required cessation of the treatment were encountered. A lower analgesic use was found in Group A.
Discussion
Ureteric colic, which is mainly due to ureterolithiasis, represents 1 to 2% of the hospital emergency admissions. There has been a significant improvement in the medical management of the ureteric calculi, with the introduction of effective medical therapeutic agents in the market. The likelihood of a ureteric stone passage is dependent on several factors, which include the stone size and the location and the ureteral conditions. Studies have shown stone passage rates between 71–98% for the distal ureteral stones which are less than 5 mm and from 25–53% for those which are between 5 and 10 mm [15]. The role of adrenergic receptors in the human ureter was first described in 1970 [16]. It was shown later that the alpha–adrenergic receptors were classified into three different subtypes of ἀ1A, ἀ1B and ἀ1D, of which the distribution in the human ureter was ἀ1D >ἀ1A >ἀ1B [17]. It was also shown that the alpha-adrenergic receptor agonists had a stimulatory effect on the ureteral smooth muscle, whereas the beta-adrenergic receptor agonists had an inhibitory effect [18]. They prevent the uncoordinated muscle activity, which is seen in renal colic, while maintaining ureteral peristalsis, which might facilitate a spontaneous stone passage [19]. The alpha blockers mainly produce relaxation of the distal human ureter by reducing the ureteric smooth muscle tone rather than completely ablating its activity. Two meta-analyses provided a high level of evidence for the clinical benefit of the alpha blockers in the patients with distal ureteral calculi, in which the patients who were given alpha blockers had 52% and 44% greater likelihoods of stone passage than those who were not given such treatment [20]. The treatment effect on the expulsion rate was partially lost, as the sizes of the stones decreased, because of the high spontaneous expulsion rate of the small stones.
Although most of the studies used tamsulosin, which is a selective a1A/a1D adrenergic receptor antagonist, the efficacies of the other alpha blockers such as Doxazosin, Terazosin, Alfuzosin and Naftopidil were also indicated [21-23]. Silodosin was approved for BPH by the US Food and Drug Administration in October 2008. Ours is perhaps one of the few studies, which has compared the efficacy between Silodosin and Tamsulosin and our results are encouraging. Regarding the incidence of the retrograde ejaculation, there is a consensus among many urologists, that its occurrence should be considered as a sign of the efficacy, rather than an adverse effect of the treatment. Silodosin appears to relax the smooth muscles of the lower urinary tract and the genital tract enough to induce a retrograde ejaculation. This was reflected in the finding that the patients who had the greatest relief from the lower urinary tract symptoms had a higher likelihood of the retrograde ejaculation. This observation suggests that the retrograde ejaculation is actually an indirect indicator of the relaxation of the smooth musculature that Silodosin induces. The same was reflected in our study, in which both the patients who had experienced the retrograde ejaculation had successfully passed the stones. The advantage of the medical expulsive therapy is important, because the risks which are related to a surgical intervention are not trivial. Studies have reported the overall complication rates after ureteroscopic lithotripsies to be 10–20%, with major complications such as ureteral perforations, avulsions and strictures occurring during 3–5% of the procedures [24]. The medical expulsive therapy should be offered as a costeffective treatment for the patients with uncomplicated lower ureteric calculi.
Conclusion
A conservative approach should be considered as an option in the management of the uncomplicated, small (≤10mm), lower ureteral stones. The findings of our study suggest that the α (1A)- adrenoceptor antagonist, Silodosin, was clinically way superior to Tamsulosin for the stone expulsion and management of these stones.
References
- Hollingsworth JM, Rogers MA, Kaufman SR, Bradford TJ, Saint S, et al. (2006) Medical therapy to facilitate urinary stone passage: a meta-analysis. Lancet 368(9542): 1171-1179.
- Trinchieri A, Ostini F, Nespoli R, Rovera F, Montanari E, et al. (1999) A prospective study of recurrence rate and risk factors for recurrence after a first renal stone. J. Urol 162(1): 27-30.
- Pak CY (1998) Kidney stones. Lancet 351(9118): 1797-801.
- Miller OF, Kane CJ (1999) Time to stone passage for observed ureteral calculi: a guide for patient education. J Urol 162(3): 688-691.
- Martin DJ, Lluel P, Guillot E, Coste A, Jammes D, et al. (1997) Comparative alpha-1 adrenoceptor subtype selectivity and functional uroselectivity of alpha-1 adrenoceptor antagonists. J Pharmacol Exp Ther 282(1): 228-235.
- Dellabella M, Milanese G, Muzzonigro G (2003) Efficiency of tamsulosin in the medical management of juxtavesicalureteral stones. J Urol 170(6): 2202-2205.
- Porpiglia F, Ghignone G, Fiori C, Fontana D, Scarpa RM (2004) Nifedipine versus tamsulosin for the management of lower ureteral stones. J Urol 172(2): 568-571.
- Tiselius HG, Ackermann D, Alken P, Buck C, Conort P, et al. (2001) Guidelines on urolithiasis. European Association of Urology 40(4): 362-371.
- Management of ureteral calculi: EAU/AUA nephrolithiasis panel. (2007) American Urological Association.
- Seitz C, Liatsikos E, Porpiglia F, Tiselius HG, Zwergel U (2009) Medical therapy to facilitate the passage of stones: what is the evidence? Eur Urol 56(3): 455-471.
- Autorino R, De Sio M, Damiano R, Di Lorenzo G, Perdonà S, et al. (2005) The use of tamsulosin in the medical treatment of ureteral calculi: where do we stand? Urol Res 33(6): 460-464.
- Borghi L, Meschi T, Amato F, Novarini A, Giannini A, et al. (1994) Nifedipine and methylprednisolone in facilitating ureteral stone passage: a randomized, double-blind, placebo-controlled study. J Urol 152(4): 1095-1098.
- Cervenàkov I, Fillo J, Mardiak J, Kopecný M, Smirala J, et al. (2002) Speedy elimination of ureterolithiasis in lower part of ureters with the alpha 1-blocker-Tamsulosin. Int Urol Nephrol 34: 25-29.
- Küpeli B, Irkilata L, Gürocak S, Tunç L, Kiraç M, et al. (2004) Does tamsulosin enhance lower ureteral stone clearance with or without shock wave lithotripsy? Urology 64(6): 1111–1115.
- Ibrahim AI, Shetty SD, Awad RM, Patel KP (1991) Prognostic factors in the conservative treatment of ureteric stones. Br J Urol 67(4): 358-361.
- Malin JM Jr, Deane RF, Boyarsky S (1970) Characterisation of adrenergic receptors in human ureter. Br J Urol 42(2): 171–174.
- Itoh Y, Kojima Y, Yasui T, Tozawa K, Sasaki S, et al. (2007) Examination of alpha 1 adrenoceptor subtypes in the human ureter. Int J Urol 14(8): 749-753.
- Weiss RM, Bassett AL, Hoffman BF (1978) Adrenergic innervation of the ureter. Invest Urol 16(2): 123-127.
- Tzortzis V, Mamoulakis C, Rioja J, Gravas S, Michel MC, et al. (2009) Medical expulsive therapy for distal ureteral stones. Drugs 69: 677-692.
- Parsons JK, Hergan LA, Sakamoto K, Lakin C (2007) Efficacy of alpha-blockers for the treatment of ureteral stones. J Urol 177(3): 983-987.
- Pedro RN, Hinck B, Hendlin K, Feia K, Canales BK, et al. (2008) Alfuzosin stone expulsion therapy for distal ureteral calculi: a double-blind, placebo-controlled study. J Urol 179(6): 2244-2247.
- Wang CJ, Huang SW, Chang CH (2008) Efficacy of an alpha1 blocker in expulsive therapy of lower ureteral stones. J Endourol 22(1): 41-46.
- Sun X, He L, Ge W, Lv J (2009) Efficacy of selective alpha1D-blocker naftopidil as medical expulsive therapy for distal ureteral stones. J Urol 181(4): 1716-1720.
- Daniels GF Jr, Garnett JE, Carter MF (1988) Ureteroscopic results and complications: experience with 130 cases. J Urol 139(4): 710-713.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...